A New Weapon in the Fight Against Prostate Cancer

Raymond Murphy, MD
The current state of prostate cancer diagnosis by TRUS biopsy is generally reliable but in a sense these biopsies are blind. Nearly 50 percent of currently detected prostate cancers may be insignificant, while 22 percent to 47 percent of saturation or template biopsies reveal cancer after an initial negative biopsy, and up to a little more than 40 percent of cancers are upgraded on final surgical pathology indicating a failure rate in detecting high-grade lesions.
Raymond Murphy, MD, PhD, a radiologist at Scottsdale Medical Imaging (SMIL), draws a hypothetically equivalent in breast cancer to make a point. “You have a blood test that tells your doctor that you probably have breast cancer,” he says. “You don’t have a mammogram, an ultrasound or an MRI to find out where it is or even which breast it is in.
Instead your doctor does 12 or maybe 24 random needle biopsies in each breast.” Murphy says that may be about to change. The combination of two technologies will bring prostate cancer diagnosis closer to that of breast cancer diagnosis.
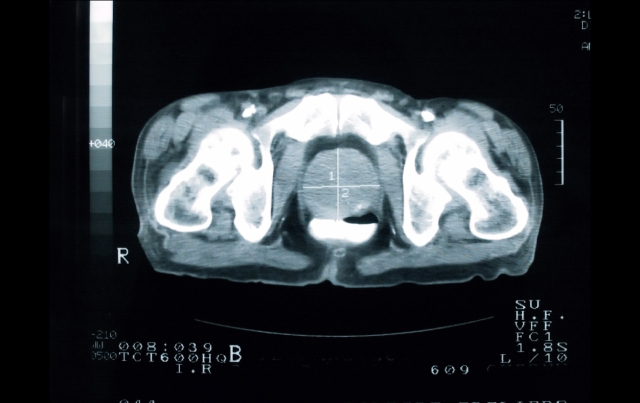
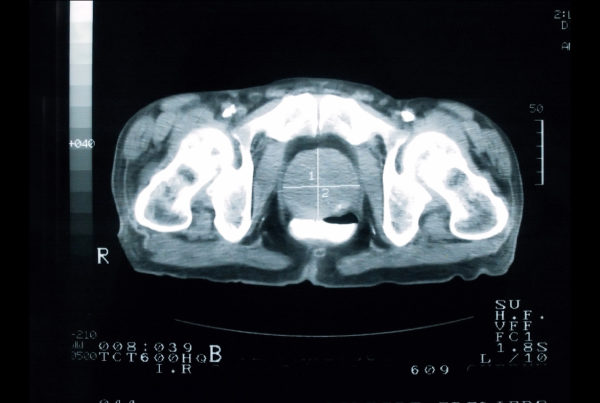
“MPMRI takes advantage of the abnormal blood flow and tightly packed cellular structure of tumors to locate, quantify and even assess the aggressiveness of prostate cancers,” Murphy says. “This noninvasive, 30-minute examination uncovers tumors in areas of the gland that are very difficult to find using standard systematic transrectal ultrasound guided biopsy technique.” While not necessary for every patient MPMRI can be used to address some specific areas of concern.
Typically used when a patient’s PSA continues to be of concern following a negative TRUS biopsy, MPMRI can help establish if the initial biopsy missed a cancer or discovered a low-grade portion of the tumor but missed a more aggressive cancer in another area of the prostate. MPMRI is also an important option when a biopsy may be difficult because of the location of the suspected tumor or in situations where a patient cannot undergo, or declines, biopsy. This technology can also be used
for continued accurate surveillance of a known tumor or a tumor that has been previously treated.
A complementary new technology, called MR-US Fusion, uses multi-parametric MRI (MPMRI) combined with new office-based MRI-ultrasound (MR-US) equipment, MR-US Fusion, marries the detailed MPMRI images with real-time ultrasound-guided biopsy images. Murphy says this will enable urologists working together with SMIL radiologists to perform targeted biopsies on even small or oddly located tumors. “MPMRI and MR-US Fusion technologies currently hold the promise of further improvement in prostate cancer diagnosis,” Murphy says, “and a future role in helping develop new therapies.”
References
Cooperberg M, Broering J, Kantoff P, et al. Contemporary trends in low-risk prostate cancer: risk
assessment and treatment. J Urol. 2007;178 (3 Pt 2):S14–S19.
Taira AV, Merrick GS, Galbreath RW, et al. Performance of transperineal template-guided mapping
biopsy in detecting prostate cancer in the initial and repeat biopsy setting. Prostate Cancer and
Prostatic Diseases. 2010;13:71-77.
Isariyawongse B, Sun L, Bañez L, et al. Significant discrepancies between diagnostic and pathologic
gleason sums in prostate cancer: the predictive role of age and prostate-specific antigen. Urology.
2008;72(4):882-886.