Evaluating Dizzy Patients

Michelle Lai Dubes, MD
Dizziness and vertigo, often accompanied by headache, imbalance or hearing loss, are frequent, challenging presenting symptoms in emergency departments (EDs).
While the majority of dizziness and vertigo are due to benign causes, a small number are due to serious conditions that, if missed, could lead to severe disability or death. This often leads to extensive neuroimaging and neurological workups.
In a study of neuroimaging usage for dizziness published last year in The Neurohospitalist, researchers found that among 907 ED patients evaluated for dizziness, 35 percent underwent neuroimaging (28 percent CT, 11 percent MRI and 4 percent both), and 20 percent had neurological consultation.
Michelle Lai Dubes, MD, a neuroradiologist at Scottsdale Medical Imaging (SMIL), says that once stroke, hemorrhage and space occupying mass are ruled out by non-contrast CT in the ED, it is often up to the primary care physician to follow up with the patient. Evaluating dizziness remains a challenge given the wide spectrum of potential causes and often poor characterization of symptoms by patients. Lai Dubes says that based on the referring physician’s assessment and clinical suspicion, SMIL’s neuroradiologists can help decide the proper course of imaging study or studies to be performed.
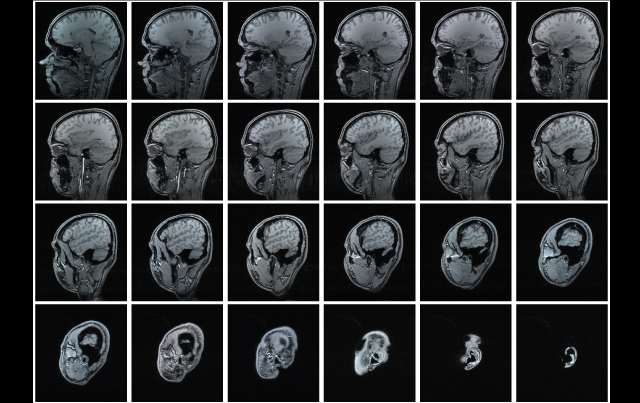
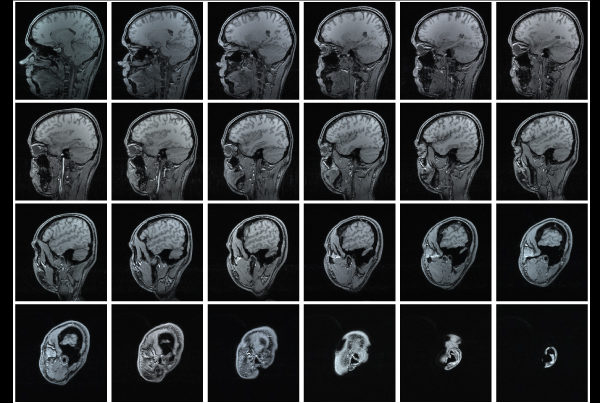
“We often recommend our IAC (internal auditory canal) protocol MRI, which utilizes intravenous contrast,” Lai Dubes says. “In addition to the routine sequences performed through the whole brain, there are additional high resolution, small field-of-view sequences performed through the temporal bones and posterior fossa to better assess the brainstem, basal cisterns, CN VII/VIII complex, the internal auditory canals and otic capsule structures.”
This type of study can detect punctate nerve sheath tumors down to 1 millimeter in size, diffuse leptomeningeal processes affecting the cranial nerves (carcinomatosis, Guillain–Barré syndrome, meningitis) and hemotympanum. In the active phase of labyrinthitis or acoustic neuritis, there may be enhancement seen within the inner ear.
If the concern is vertebrobasilar insufficiency, MRA of the head and neck is recommended. In select cases, this could be followed up with CTA and/or temporal bone CT. “A significant majority of outpatient imaging studies performed for workup of dizziness, however, have no imaging cause
identified,” Lai Dubes says. “These include migraines, BPPV, Meniere’s disease, orthostatic hypotension and pharmacologically induced symptoms.”
References
Navi B, Kamel H, Shah M, et al. The use of neuroimaging studies and neurological consultation to
evaluate dizzy patients in the emergency department. The Neurohospitalist. 2012;7-15.