SMIL moves quickly to add NETSPOT® for NETs diagnostic imaging
With the growing incidence of neuroendocrine tumors (NETs) and the significant differential in 5-year survival depending on early vs. late diagnosis, diagnostic imaging’s role in the identification and treatment of these rare tumors has taken on greater urgency.

Nishant Verma, MD
With that backdrop, Scottsdale Medical Imaging has moved quickly to be among the first in the Southwest to offer Gallium-68 DOTATATE (NETSPOT®) imaging to provide greater confidence in the early diagnosis of NETs.
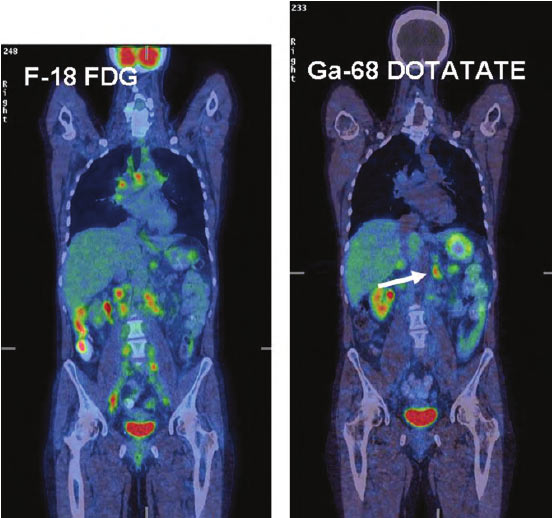
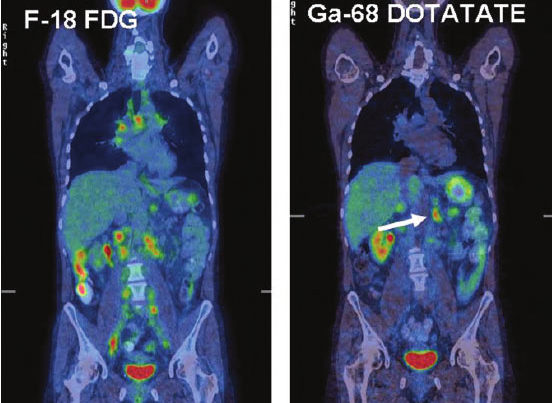
Nuclear Medicine specialist Nishant Verma, MD, of Scottsdale Medical Imaging (SMIL), says NETSPOT offers significantly higher sensitivity for somatostatin receptor positive neuroendocrine tumors than octreotide and combined with PET and CT imaging provides higher resolution images that can identify much smaller lesions.
“By targeting and binding to the somatostatin receptor via the dotatate peptide and emitting low-level radiation via the Ga 68 radioisotope, NETSPOT® combined with PET produces a much higher resolution image than was possible with octreotide scan, allowing us to see even smaller lesions” Dr. Verma said. “With its lower effective radiation dose together with much simpler preparation compared to octreotide scan, NETSPOT® imaging is a superior diagnostic choice for NETs.”
Dr. Verma added that NETSPOT has 100 times higher affinity for somatostatin receptor type 2 than octreoscan, which significantly improves detection. As a result oncologists have a clearer picture of disease extent on which to base surgery vs. systemic therapy recommendations.
In a 2016 Journal of Nuclear Medicine study of safety and efficacy in 78 patients with known or suspected pulmonary or gastroenteropancreatic neuroendocrine tumors, researchers found that Ga-DOTATATE PET/CT combined with CT or liver MRI changed care in 28 of 78 (36%) patients. The researchers concluded that with improved accuracy, little toxicity and lower radiation exposure, “Ga-DOTATATE [NETSPOT®] imaging should be used instead of In-pentetreotide [Octreoscan] imaging where available.”
In addition, standardized uptake value analysis of Ga-DOTATATE has been shown to be predictive of progression-free survival following peptide receptor radionuclide treatment (PRRT) and was associated with an improvement in clinical symptoms among patients with well-differentiated neuroendocrine tumors.
With FDA approval of NETSPOT® for adult and pediatric patients in 2016, the advanced imaging quality quickly gained NETSPOT® inclusion in the National Comprehensive Cancer Network’s guidelines and has been granted Transitional Pass-Through status by the Centers for Medicare and Medicaid Services.
Dr. Verma says given the research evidence, SMIL believes NETSPOT® combined with PET/CT offers referring physicians superior diagnostic confidence compared with the former standard of somatostatin receptor scintigraphy (SRS) and will offer patients earlier diagnosis with better outcomes.
In short, PET/CT imaging with NETSPOT® provides earlier, surer diagnosis for patients with NETS and early diagnosis is associated with significantly better survival.
Deppen SA, Liu E, Blume JD, et al. “Safety and efficacy of 68GA-DOTATATE PET/CT for diagnosis, staging and treatment of neuroendocrine tumors,” J Nucl Med. 115.163865 2016;doi:10.2967/jnumed. Epub ahead of print.
Haug et al; “68Ga-DOTATATE PET/CT for the Early Prediction of Response to Somatostatin Receptor–Mediated Radionuclide Therapy in Patients with Well-Differentiated Neuroendocrine Tumors,” J Nucl Med September 1, 2010 vol. 51 no. 9 1349-1356
Deppen SA, Liu E, Blume JD, et al. “Safety and efficacy of 68GA-DOTATATE PET/CT for diagnosis, staging and treatment of neuroendocrine tumors,” J Nucl Med. 115.163865 2016;doi:10.2967/jnumed. Epub ahead of print.
Haug et al; “68Ga-DOTATATE PET/CT for the Early Prediction of Response to Somatostatin Receptor–Mediated Radionuclide Therapy in Patients with Well-Differentiated Neuroendocrine Tumors,” J Nucl Med September 1, 2010 vol. 51 no. 9 1349-1356